The science behind drug detoxification is a complex interplay of physiology and neurochemistry. As the body works to purge itself of harmful substances, it undergoes extensive changes, marked by physical discomfort and emotional turbulence. This process, while critical in the journey towards recovery, requires careful medical supervision to manage withdrawal symptoms and prevent potential complications. What exactly happens in the body during detox? And how do we navigate the tumultuous aftermath to restore health and resilience? These are intricate questions that deserve our exploration.
Understanding the Detox Process
To fully comprehend the science behind drug detoxification, one must first understand the detox process in detail. The process involves the body systematically eliminating harmful substances, specifically drugs or toxins, which can cause significant physiological changes. The detox process can be facilitated through several detoxification methods, often including medically supervised withdrawal. This ensures that the patient’s health is safeguarded during the potentially dangerous detox process. The success primarily hinges on the physiological changes that occur within the body, which are the body’s natural response to the absence of substances it has become accustomed to.
When drugs are introduced into the body, they alter the brain’s functioning and the body’s overall balance. The detox process aims to restore this balance, often causing temporary but intense side-effects. In contrast, outpatient detoxification methods allow the patient to detox at home with regular check-ups, enabling them to maintain some level of normalcy in their daily lives. These changes are crucial to understanding the broader picture of drug detoxification.
The Body’s Response to Withdrawal
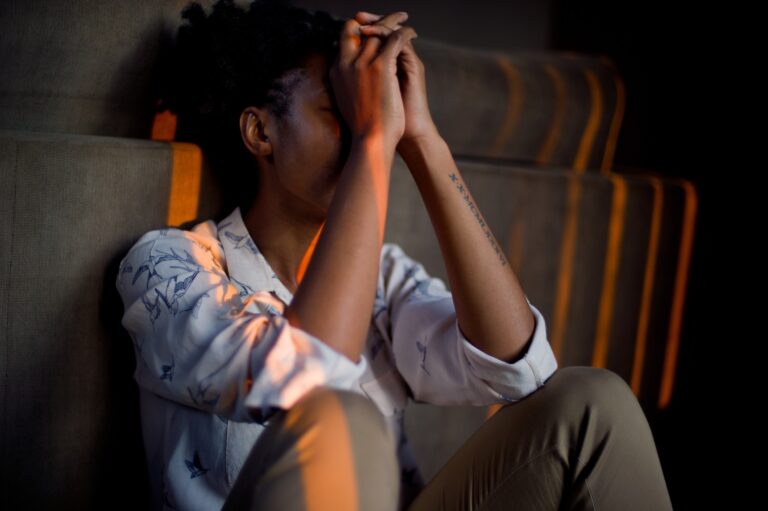
Having thoroughly examined the detox process, we can now turn our attention to a significant aspect of detoxification – the body’s response to withdrawal. This phase is characterized by a series of withdrawal symptoms, which are the physical and psychological responses to the sudden cessation or reduction of substance use. These symptoms can range from mild such as anxiety, restlessness, and irritability, to severe – including seizures, hallucinations, and even death in extreme cases. The intensity and duration of these symptoms vary widely, influenced by factors such as the type of substance used, the duration and intensity of use, and individual health status.
What drives these withdrawal symptoms are the profound neurochemical changes occurring in the brain. With habitual drug use, the brain adapts to the constant presence of the substance by altering its chemical balance. This is an attempt to maintain a state of equilibrium or ‘normalcy’. However, when the substance is abruptly withdrawn, the brain struggles to readjust, leading to the manifestation of withdrawal symptoms. Understanding the body’s response to withdrawal is essential as it not only dictates the immediate medical care required but also shapes the long-term treatment strategy. It underscores the importance of medical supervision during detoxification, ensuring safety and enhancing the chance of successful recovery.
Healing and Recovery: The Aftermath
In the aftermath of detoxification, the focus shifts to healing and recovery, a vital period that often determines the success or failure of the entire process. This phase involves both physical and psychological healing, allowing the body and mind to regain balance and stability following the storm of detoxification. Physical healing post detox often involves reestablishing healthy nutrition, exercise, and sleep patterns. Emotional resilience, on the other hand, is often fostered through therapy and support groups. Cognitive-behavioral therapy can equip individuals with the skills needed to manage stress and negative emotions without resorting to substance use.
Post detox wellness is a multifaceted concept, involving not only physical healing but also the cultivation of emotional resilience. It’s during this period that the body’s natural healing mechanisms work to repair the damage inflicted by substance abuse. Nutritional therapy, for instance, can replenish the nutrients lost during prolonged substance abuse, helping the body regain strength and combat fatigue. Support groups provide a community of individuals who share similar experiences, offering mutual support and understanding that can be vital for maintaining motivation during the recovery journey.
Final Thoughts

At Altitude Recovery, we’re here to elevate you from the challenges of substance use to a place of lasting resilience and renewal. Our dedicated team crafts personalized, evidence-based treatment plans, guiding you on a journey uniquely tailored to your needs and goals. Reach out for the compassionate support you deserve on your path to wellness by contacting us. Follow us on Facebook for more insights, resources, and stories of hope as we walk alongside you towards recovery.
Frequently Asked Questions
How Do Different Types of Drugs Affect Detox Timeframes?
Detox timeframes vary greatly depending on the type of drug. Opioid withdrawal, for instance, can last from a week to a month. Alcohol metabolism is relatively quick, with detox typically lasting up to a week. Stimulant clearance, like cocaine, can take several days to a week. Conversely, benzodiazepines have lingering effects, with detox potentially taking several weeks. Factors such as usage frequency, dosage, and individual health also influence these timelines.
What Role Do Genetics Play in Drug Detoxification?
Genetic variations substantially impact drug detoxification. Individual genes influence the functioning of detox pathways, modulating the pace and efficiency of drug metabolism and elimination. Certain genetic profiles can expedite detoxification, while others may slow the process, leading to increased susceptibility to adverse drug effects. Understanding these genetic influences allows for personalized treatment strategies, optimizing detoxification processes and reducing potential risks.
How Does Age and Overall Health Condition Affect the Detox Process?
Age and overall health considerably affect the detoxification process. Age factors influence the body’s metabolic speed, affecting how quickly substances are eliminated. Health influences such as pre-existing conditions or compromised immune systems can slow the detox process, making it more challenging. A strong, healthy individual may detoxify more efficiently than someone with poor health or advanced age, as their body can better manage the physical stress of detoxification.
Are There Specific Diets or Foods That Can Aid in Drug Detoxification?
Yes, certain diets and foods can aid in drug detoxification. Nutritional strategies, such as a diet rich in fruits, vegetables, lean proteins, and whole grains can support the body’s natural detoxification process. Foods high in fiber aid in eliminating toxins through the digestive tract. Adequate hydration and inclusion of detoxification foods like garlic, ginger, and beetroot, which boost liver function, can also expedite the detox process.
Can Mental Health Conditions Impact the Effectiveness of Drug Detox?
Yes, mental health conditions can greatly impact the effectiveness of drug detox. Such conditions may exacerbate withdrawal symptoms, complicating the detox process. For instance, anxiety or depressive disorders can intensify feelings of discomfort and cravings. Consequently, a thorough detox strategy should consider mental health status, ensuring the provision of necessary therapeutic support alongside physical detoxification. Ultimately, successful detox requires addressing both physical dependency and mental health aspects.